A Remarkable Stroke Recovery: A Case Study of Mechanical Thrombectomy
By:

Dr. Lalit Kumar Bhardwaj

Dr. Navneet Agarwal
02-02-2024 5 Min Read

Explore the mysterious world of neurology as we delve into this case study about dealing with a severe ischemic stroke. This kind of stroke happens when blood flow to a part of the brain gets blocked, causing damage to the tissues of the brain. Follow along as we share the unsettling experience of a previously healthy 30-year-old man who now faces sudden sensory changes and mild right-side weakness.
Clinical Presentation
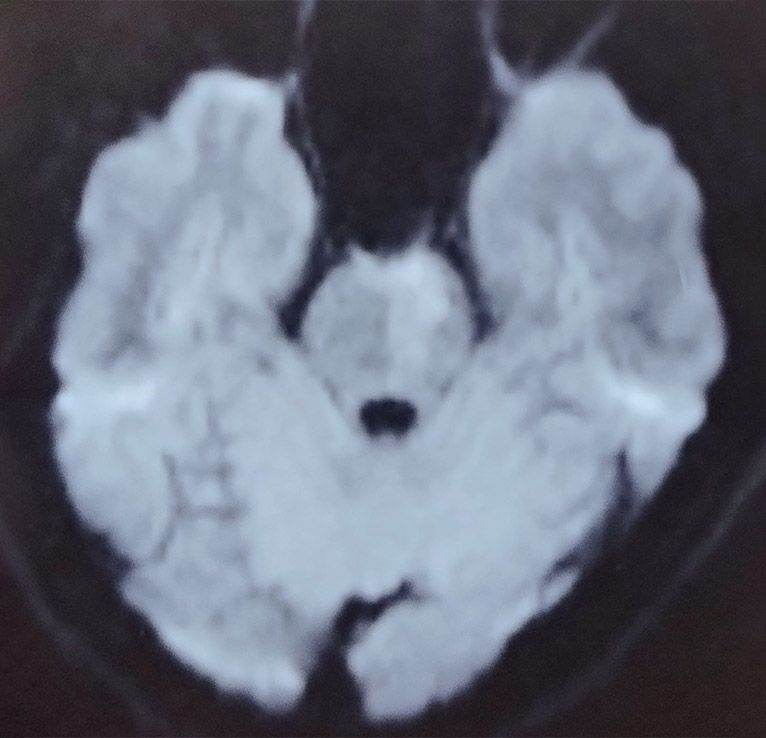
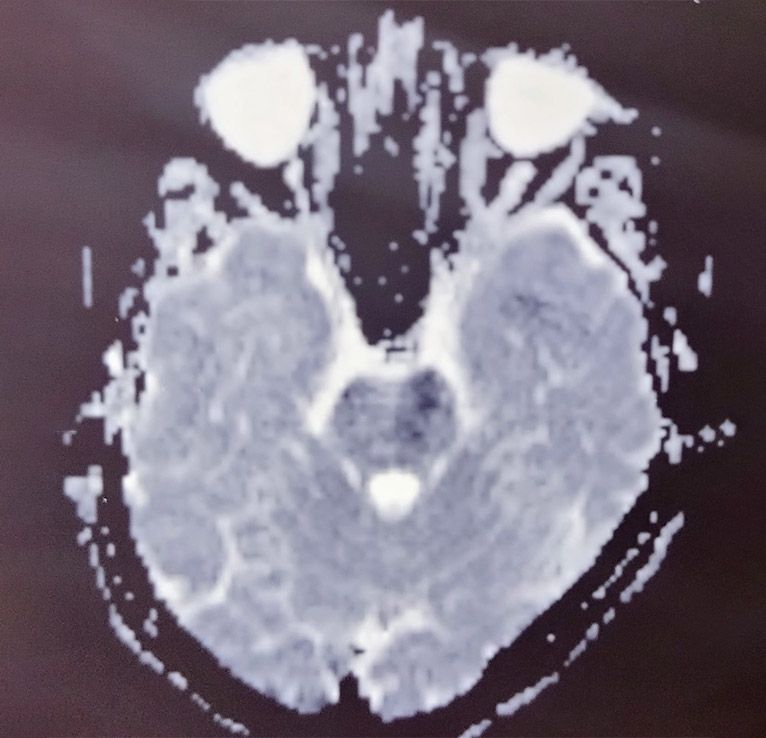
Our patient, a 30-year-old man with no notable medical issues, arrived at our hospital experiencing a sudden change in consciousness and a bit of weakness on his right side. The MRI results revealed concerning damage in the left side perforator territory, indicating potential issues with blood flow and setting the stage for a challenging medical situation.
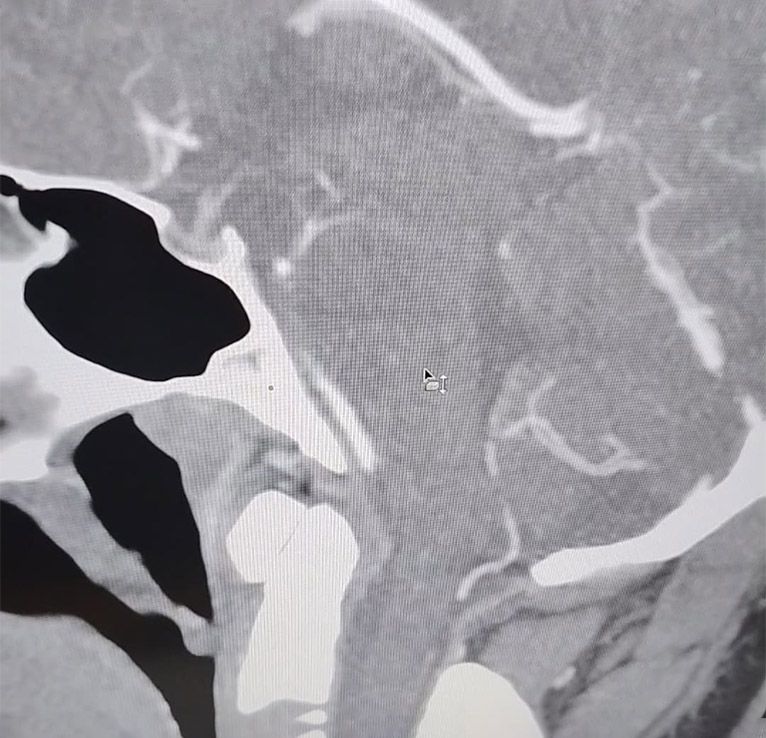
Following a later CT angiogram, we discovered a troubling situation. There was insufficient blood flow in the lower part of the Basilar artery, which was unexpected given the seemingly good flow in both the Superior Cerebellar Artery (SCA) and Posterior Cerebral Artery (PCA). In line with the acute ischemic stroke protocol, we started a process that unfortunately led us into a situation where the condition of the patient kept worsening.
Challenges and Deterioration:
Even though we made efforts to follow the acute ischemic stroke protocol, the patient's situation kept getting worse. The person became excessively drowsy, had difficulty responding to speech, and the weakness on the right side increased to a 3/5 scale, creating a grim picture. Feeling the urgency—or maybe giving in to despair—we chose to do Cerebral Digital Subtraction Angiography (DSA) under general anaesthesia, along with Mechanical Thrombectomy.
Procedure and Risk-Benefit Analysis:
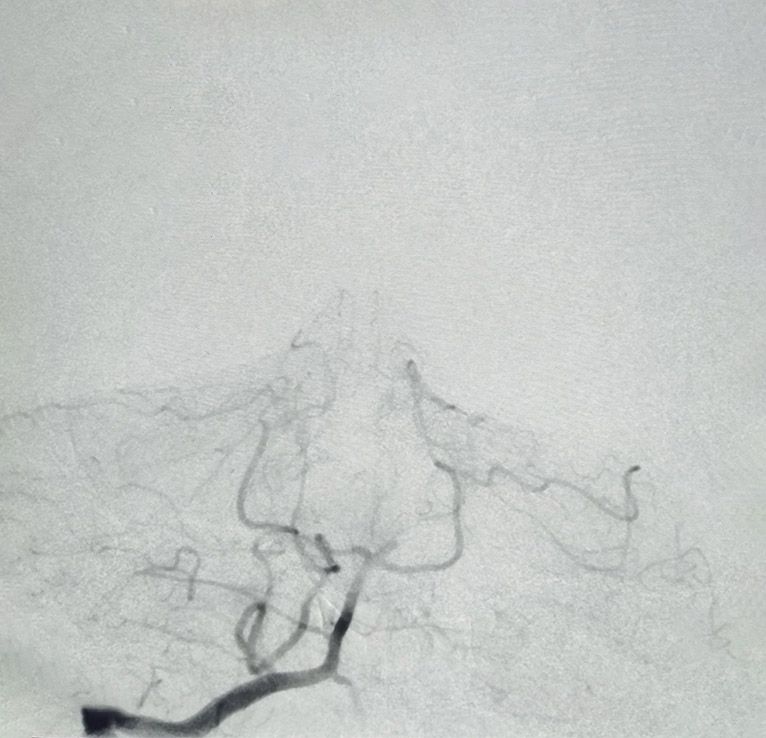
Choosing to go ahead with DSA and Mechanical Thrombectomy felt like taking a significant risk. Before the procedure, we only partially explained the possible risks and benefits to the patient. The images from the DSA before the procedure showed a troubling scene—hardly any blood flow in the left PCA, and the right PCA looked like a fatal pattern, signalling a sense of impending doom.
Post-Procedure Catastrophe:
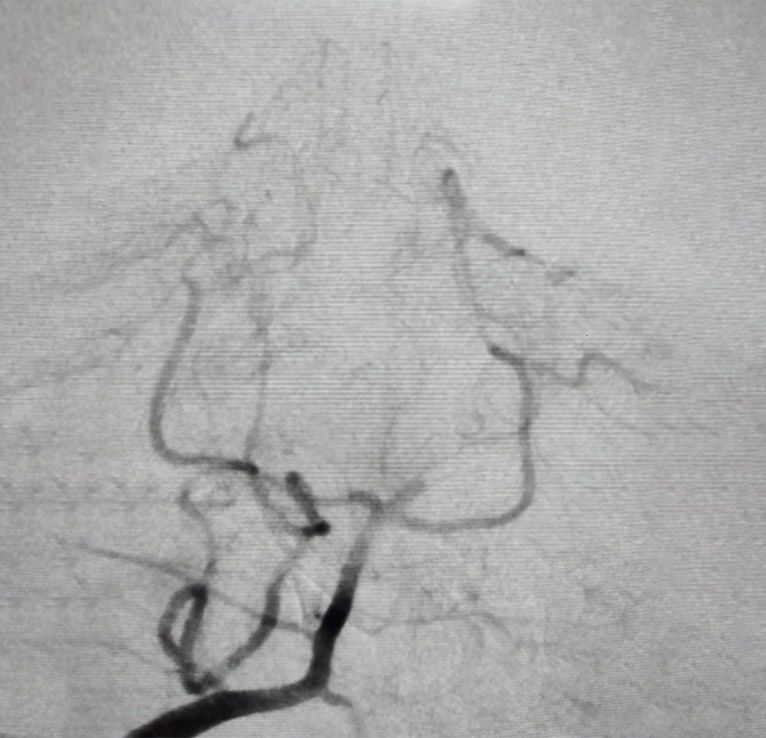
We opted to go ahead with mechanical thrombectomy. The use of Mechanical Thrombectomy turned out to be a crucial moment in this case. After the procedure, DSA images showed a different narrative—the left PCA opened, and there was a restored flow in the suitable PCA from the posterior circulation, a miraculous turn in this medical tragedy. The patient's impressive recovery journey continued along a path of ongoing challenges.
Discharge and Never-Ending Nightmare:
After a hospital stay of 5 days, the patient underwent a remarkable transformation from a living nightmare. The recovery was astonishing, fully conscious and cooperative, with a GCS of 15, everyday speech, and no apparent cranial neuropathy. The removal of the nasogastric tube indicated improved swallowing function, and though some assistance was still required for walking, the overall progress seemed miraculous.
Conclusion
This case underscores the importance of swift and decisive action in acute ischemic stroke scenarios. The collaboration between medical management, interventional procedures, and comprehensive patient care can yield remarkable outcomes. As we celebrate the success in this particular case, it serves as a reminder of the strides we continue to make in the field of neurology and the hope we can offer to patients facing challenging neurological conditions.
FAQS
Related Articles
Connect With Us
Health In A Snap, Just One App.
KNOW MORE

























































































































































