Spondyloarthropathies

What is Spondylarthritis?
Spondylarthritis (SpA) is not a single disease but a family of inflammatory conditions that primarily affect the spine and joints where your spine connects to the pelvis, especially the sacroiliac joints. The term itself comes from “spondylo” (meaning spine) and “arthritis” (joint inflammation). One of the most common early signs of spondylarthritis is chronic lower back pain, especially in younger adults.
But SpA doesn’t stop at the spine, it can also impact joints in your arms and legs, your eyes, skin, and even the digestive tract.
Unlike osteoarthritis (which is caused by wear and tear) or rheumatoid arthritis (an autoimmune condition), spondylarthritis is its category of inflammatory arthritis. It is typically autoimmune, meaning the body’s immune system mistakenly attacks its own tissues, especially joints and connective tissues.
Here are some defining features:
- Inflammatory and Rheumatic
SpA is a rheumatic disease, which means inflammation, not mechanical damage, is the main driver of joint pain, stiffness, and swelling. This type of arthritis often begins before age 45 and tends to be chronic and progressive.
- Seronegative Arthritis
SpA is considered “seronegative” because patients don’t test positive for rheumatoid factor (an antibody often seen in RA). That’s why doctors sometimes use the term “seronegative spondyloarthropathy.”
- Enthesitis: A Key Symptom
One hallmark of SpA is enthesitis, inflammation at the points where tendons and ligaments attach to bones, called entheses. This can cause localized pain, especially in the heels, knees, and elbows.
- Genetic Links: HLA-B27
A significant number of people with SpA, particularly of Northern European descent, carry a gene called HLA-B27. While having this gene doesn’t guarantee you’ll develop SpA, it does increase your risk and can support diagnosis when symptoms are present.
Types of Spondylarthritis
Treatment options
Spondylarthritis doesn’t have a one-size-fits-all treatment, and it currently has no cure. But with the right care, many people can manage their symptoms effectively and continue leading full, active lives. The goal of treatment is simple: ease pain, reduce inflammation, preserve mobility, and prevent long-term joint damage.
Doctors usually take a step-by-step approach, starting with the most conservative options and adjusting based on how your symptoms respond.
Initial Treatments
- Low-impact exercise: Movement might feel uncomfortable at first, but it’s essential. Regular physical activity helps reduce stiffness, strengthen muscles, and improve flexibility.
- NSAIDs (nonsteroidal anti-inflammatory drugs): Over-the-counter medications like ibuprofen or naproxen can help relieve pain and decrease inflammation.
When Symptoms Persist
- Corticosteroid Injections
- DMARDs (Disease-Modifying Anti-Rheumatic Drugs)
- Traditional DMARDs (like methotrexate)
- Biologic DMARDs, which include TNF-alpha blockers and IL-17 inhibitors, are often used when inflammation is widespread or persistent.
If your pain or inflammation remains stubborn, your doctor may explore more targeted treatments:
For localized pain, particularly in specific joints or areas with enthesitis, occasional cortisone shots can provide relief.
These are more advanced medications designed to slow the progression of inflammation rather than just treat symptoms. They come in two forms:
Condition-Specific Approaches
Some forms of spondylarthritis, like psoriatic arthritis or enteropathic arthritis, may require treatments tailored to the underlying conditions, such as psoriasis or inflammatory bowel disease. Your doctor will coordinate care with other specialists if needed.
Supportive and Preventive Care
- Physical therapy is a cornerstone of most treatment plans. A trained therapist can design exercises tailored to your needs, helping improve strength, balance, and posture.
- Smoking cessation is strongly recommended. Smoking can worsen inflammation and reduce the effectiveness of medications. If you smoke, talk to your doctor about supportive ways to quit — there are programs and resources designed to help you succeed.
- Antibiotics may be used if your spondylarthritis stems from a bacterial infection, such as in reactive arthritis.
Surgery is rarely needed, but in severe cases, where joints are severely damaged, procedures like joint replacement or repair may be considered.
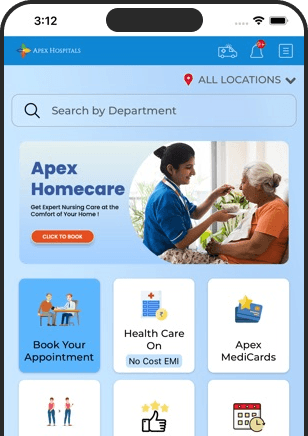
At Apex Hospitals, we understand that spondylarthritis affects more than just your joints — it impacts your daily life, mobility, and overall well-being. That’s why our team of experienced rheumatologists and physiotherapists takes a personalized, holistic approach to treatment. From advanced diagnostics to tailored therapy plans, we’re here to support you every step of the way.
Whether you're just starting your journey with spondylarthritis or looking to optimize your current treatment plan, Apex Hospitals is committed to helping you live with less pain and more freedom. Your health, comfort, and mobility are our top priorities — because you deserve to move through life with strength and support.
Let us help you take the next step toward better joint health and a better quality of life.
FAQS
Health In A Snap, Just One App.
KNOW MORE