What is Lupus?
- Infections
- Certain medications
- Sunlight exposure
Lupus is an autoimmune condition, meaning the body's immune system, which is supposed to defend against illness, mistakenly attacks its healthy tissues and organs. This internal conflict can lead to widespread inflammation that may affect the joints, skin, kidneys, heart, lungs, brain, and blood cells.
One of lupus's biggest challenges is its unpredictability. Its symptoms mimic many other conditions, making diagnosis notoriously difficult. Among its more recognizable features is a butterfly-shaped rash that appears across the cheeks and nose, but not everyone with lupus experiences this sign.
The exact cause of lupus isn't fully understood, but a mix of genetic predisposition and environmental triggers plays a role. For some, lupus may be activated by:
Interestingly, some people may carry a genetic tendency for lupus their whole lives and never develop the disease unless it's triggered by one of these factors.
Lupus isn't a single disease but a family of conditions that impact the body differently. Systemic Lupus Erythematosus (SLE) is the most common form, which affects multiple organs and systems. Because of its wide-reaching impact, SLE is typically what people mean when discussing lupus.
Types of Lupus
1. Systemic Lupus Erythematosus (SLE)
This type is characterized by inflammation that can impact multiple systems in the body, including the skin, joints, kidneys, heart, lungs, brain, and blood. SLE can range from mild to life-threatening, and symptoms often appear in cycles, with flares followed by periods of remission. Fatigue, joint pain, and skin rashes are common, but the condition is highly individual, with some people experiencing more severe organ involvement.
2. Cutaneous Lupus
It primarily affects the skin and manifests as rashes, lesions, or discolouration, particularly in sun-exposed areas. There are subtypes within this category: chronic cutaneous lupus, also known as discoid lupus, leads to round, scarring rashes; subacute cutaneous lupus causes red, scaly, ring-shaped patches; and acute cutaneous lupus often results in the classic "butterfly rash" over the cheeks and nose. While cutaneous lupus mainly affects the skin, in some cases, it may develop into systemic lupus.
3. Drug-Induced Lupus Erythematosus
It is another form of the disease that arises as a side effect of certain prescription medications, such as hydralazine, procainamide, or isoniazid. The symptoms often resemble those of SLE, including joint pain and fatigue, but they tend to be less severe and typically resolve once the triggering medication is discontinued. This type usually does not involve the organs as deeply as systemic lupus.
4. Neonatal Lupus
It is a much rarer form that affects newborns. It occurs when a mother with lupus or lupus-related antibodies passes these antibodies to her baby during pregnancy. The infant may be born with skin rashes, liver issues, or low blood cell counts. In most cases, the symptoms disappear within a few months, but in rare instances, it can lead to a serious heart condition known as congenital heart block, which may require a pacemaker.
Lastly, lupus can sometimes be confined to a specific body part. These organ-specific manifestations are often classified under the umbrella of SLE. Still, they may be referred to more specifically, such as lupus nephritis, which affects the kidneys, or CNS lupus, which targets the brain and nervous system. These cases require specialized management due to the critical nature of the organs involved.
Treatment options
Managing lupus involves a combination of medication, lifestyle changes, and supportive therapies to control symptoms, reduce inflammation, and protect organs from long-term damage. Since lupus affects individuals differently, treatment is personalized based on symptoms, disease severity, and organ involvement.
Medical Treatments
1. Hydroxychloroquine
This is one of the most commonly prescribed medications for lupus. It’s a disease-modifying antirheumatic drug (DMARD) that helps reduce flares, control symptoms like joint pain and rashes, and slow down disease progression. Many people with lupus take it long-term.
2. Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
NSAIDs like ibuprofen can ease joint pain, muscle aches, and inflammation. They're available over the counter, but long-term use should always be monitored by a healthcare provider.
3. Corticosteroids
These powerful anti-inflammatory medications are often used during lupus flares. However, they are typically used for short durations to avoid side effects.
4. Immunosuppressants
For moderate to severe lupus, these drugs may be used to suppress the immune system. These are often necessary when lupus affects internal organs like the kidneys or brain.
5. Biologic Drugs
It works by targeting specific immune cells, helping to reduce flares and disease activity.
6. Additional Treatments
Depending on how lupus affects the body, additional treatments may be needed. These can include medications for:
Osteoporosis
Seizures or kidney complications
- Sun Protection
- Balanced Diet
- Increase omega-3 fatty acids (found in fish, flaxseeds, walnuts)
- Reduce cholesterol and saturated fats
- Limit salt intake to manage blood pressure
- Regular Exercise
- Stress Management
- Quit Smoking
- Limit Alcohol
Lifestyle and Home Remedies
In addition to medical treatment, several lifestyle choices can help reduce lupus symptoms and improve quality of life.
Sunlight can trigger lupus flares. Wearing protective clothing, wide-brimmed hats, and using broad-spectrum sunscreen is essential for skin protection.
While there’s no special "lupus diet," certain dietary choices can support overall health:
Ensure adequate vitamin D and B intake
Consulting our dietitians can help you create a personalized nutrition plan.
Gentle, low-impact activities like walking, swimming, and yoga can help maintain joint flexibility, reduce fatigue, and support cardiovascular health.
Emotional stress can worsen symptoms. Practices like meditation, journaling, deep breathing, or joining a support group can help keep stress in check.
Smoking increases inflammation and can worsen lupus symptoms. If you smoke, your healthcare provider can guide you toward resources for quitting.
Alcohol can interfere with medications and worsen side effects. It’s best to limit or avoid it altogether.
Living with lupus can be challenging, but with the proper care, support, and lifestyle changes, it is possible to lead a fulfilling life. Apex Hospitals is committed to providing comprehensive and compassionate care for individuals with lupus and other autoimmune conditions. Our team of experienced rheumatologists ensures that every patient receives the personalized attention they deserve. Whether you're newly diagnosed or navigating long-term management, Apex Hospitals is here to support you every step of the way.
FAQS
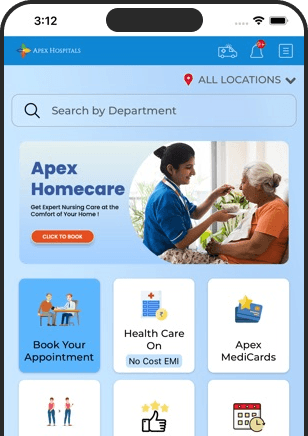
Health In A Snap, Just One App.
KNOW MORE