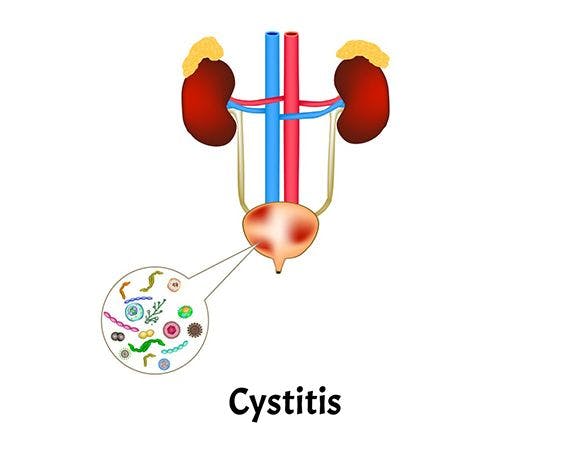
What is interstitial cystitis (IC)?
Interstitial cystitis (IC), also known as painful bladder syndrome, poses a diagnostic challenge and lacks a definitive cure. Its diverse symptoms and varying severity lead experts to consider it a spectrum of related diseases. If you experience urinary pain persisting for more than six weeks, unrelated to conditions like infection or kidney stones, IC may be the cause. Despite its impact on social life, exercise, sleep, and work, there are treatments available to manage symptoms and empower individuals with the knowledge to navigate life with IC effectively.
Who can get interstitial cystitis (IC)?
Interstitial cystitis (IC) predominantly affects women, with approximately 90% of those diagnosed being female. Around 3% to 6% of adult women, totalling an estimated 3 to 8 million in the United States, experience some form of IC. Additionally, about 1.3% of American men are affected by this condition. Typically, individuals begin facing IC-related challenges in their 40s, and the risk of developing it increases with age.
Treatments
Home or Lifestyle Treatments
For approximately half of interstitial cystitis cases, the condition may resolve independently. However, for those requiring treatment, symptom management is the primary focus. Discovering the most practical combination of treatments often involves trial and error, with relief typically taking weeks or months.
The initial stage of treatment aims to avoid triggers and implement lifestyle changes to alleviate symptoms. Some home or lifestyle treatments include:
1. Bladder Retraining: Gradually extend the time between bathroom breaks to increase bladder capacity.
2. Stress Reduction: Minimize stress through stretching, reading, relaxation techniques, talking to friends, or meditation.
3. Comfortable Clothing: Wear loose-fitting clothes to avoid unnecessary pressure on the bladder.
4. Low-Impact Exercise: Engage in low-impact exercises like walking or stretching.
5. Dietary Changes: Modify your diet to eliminate potential triggers. Common triggers include citrus fruits, tomatoes, chocolate, caffeinated drinks, carbonated drinks, alcohol, spicy foods, and artificial sweeteners. Keeping a food and symptom journal can help identify connections.
6. Smoking Cessation: Quit smoking, as it may contribute to symptoms.
Individuals may find that certain foods or drinks exacerbate their symptoms, and an elimination diet, guided by a healthcare professional, can help identify specific triggers affecting the bladder. Consult with our expert urologists in Jaipur for personalized guidance and support.
Second Line Treatment
If lifestyle changes prove insufficient in managing interstitial cystitis, the following line of treatments may be considered:
1. Physical Therapy: Various techniques help relax pelvic muscles and alleviate symptoms.
2. Amitriptyline: This medication controls bladder spasms and is the most commonly prescribed oral medication for IC.
3. Pentosan (Elmiron): While the exact mechanism is unclear, this drug may aid in rebuilding the lining of the bladder tissue. It may take a few months to see symptom relief.
4. Hydroxyzine: An antihistamine, this drug can be beneficial for individuals experiencing frequent nighttime urination.
5. Dimethyl Sulfoxide (DMSO): DMSO is instilled into the bladder using a catheter for those who haven't found relief with other medications. It is believed to combat inflammation and block pain. However, doctors may not often recommend it due to the potential temporary worsening of symptoms and the need for multiple visits.
These second-line treatments offer additional options for managing interstitial cystitis and can be discussed with our expert urologists to determine the most suitable approach for individual cases.
Third line treatment
Suppose second-line treatments prove ineffective for interstitial cystitis. In that case, the medical approach may progress to third-line treatments, often requiring cystoscopy—a specialized procedure to examine the bladder, typically performed in an operating room under anaesthesia. If necessary, a referral to a urologist specializing in bladder issues may be recommended.
Bladder Stretching: Gradually stretching the bladder wall with fluid may relieve symptoms. If effective, the results usually last less than six months, and repeat treatments may be considered.
Steroids: For individuals with ulcers known as Hunner’s lesions on the bladder, a doctor may opt for removal, cauterization, or steroid injections.
Fourth Line treatment
In cases where lifestyle adjustments, medications, and the procedures above fail to address symptoms significantly, and the patient's quality of life is substantially impacted, urologists may explore fourth-line treatments:
1. Neurostimulation involves the implantation of a device that delivers tiny electrical shocks to nerves, altering their function.
2. OnabotulinumtoxinA (Botox) Injections: Temporary paralysis of the bladder muscle using Botox injections to alleviate pain.
Fifth Line treatment
When these interventions are insufficient and symptoms persist, the following options may be considered:
1. Cyclosporine: An immunosuppressive drug to modulate the immune system.
2. Surgery: Reserved for sporadic cases where all other treatments prove ineffective, involving a complex operation redirecting urine away from the bladder.
In instances where conventional IC treatments yield limited success, pain management strategies, such as painkillers, acupuncture, or alternative approaches, may be explored to mitigate symptoms.
Speak to our experts about interstitial cystitis (IC).
If you're seeking guidance or information about interstitial cystitis (IC), our experts are here to help. Whether you have questions about symptoms or treatments or want to discuss your situation, our team is dedicated to providing valuable insights and support. Please feel free to reach out, and we'll do our best to assist you on your journey with interstitial cystitis.
FAQS
Health In A Snap, Just One App.
KNOW MORE