Sickle cell anemia
What is sickle cell anemia?
Sickle cell anemia is a hereditary condition under the umbrella term of sickle cell disease. This disorder alters the typical shape of red blood cells that transport oxygen throughout the body.
Ordinarily, red blood cells are circular and flexible, allowing them to navigate blood vessels smoothly. In sickle cell anemia, however, some red blood cells adopt a sickle or crescent shape. These aberrant cells also become stiff and adhesive, potentially obstructing or slowing blood flow.
Current treatment strategies focus on alleviating pain and minimizing the risk of disease-related complications. Nevertheless, ongoing research into newer treatments holds promise for potentially curing individuals affected by this condition.
What are the causes of sickle cell anemia?
Sickle cell anemia arises from a genetic mutation affecting the gene responsible for hemoglobin production. Hemoglobin is the crucial iron-rich compound within red blood cells that facilitates oxygen transport from the lungs to various tissues in the body. In sickle cell anemia, the altered hemoglobin forms rigid, adhesive, and distorted red blood cells.
For a child to inherit sickle cell anemia, both parents must carry one copy of the sickle cell gene and transmit both to the child.
If only one parent transmits the sickle cell gene, the child will have the sickle cell trait. Individuals with the sickle cell trait possess one normal hemoglobin gene and one sickle cell gene. As a result, they produce both standard and sickle cell hemoglobin. While their blood may contain some sickle cells, they typically remain asymptomatic. However, they are carriers of the disease and can pass the gene to their offspring.
What are the risk factors of sickle cell anemia?
Children are susceptible to sickle cell disease only if both parents carry the sickle cell trait. Additionally, a blood examination known as hemoglobin electrophoresis can ascertain the specific type an individual holds.
Individuals hailing from regions endemic to malaria are more prone to being carriers. These regions encompass:
- Africa
- India
- Mediterranean regions
- Saudi Arabia
What are the symptoms of sickle cell anemia?
Symptoms of sickle cell anemia typically emerge around 6 months of age and can vary among individuals, evolving. These symptoms may include:
1. Anemia: Sickle cells have a shorter lifespan than normal red blood cells, leading to a deficiency known as anemia. This shortage of red blood cells results in insufficient oxygen delivery to the body, causing fatigue.
2. Episodes of pain: Intermittent and severe pain crises caused by the blockage of blood flow by sickle-shaped red blood cells are a hallmark symptom. These painful episodes can affect the chest, abdomen, and joints, varying in intensity and duration from a few hours to several days. Some individuals experience frequent crises, necessitating hospitalization.
3. Swelling of hands and feet: Impaired blood circulation due to sickle cell blockage can lead to swelling in the extremities.
4. Frequent infections: Sickle cell damage to the spleen compromises its function in fighting infections, increasing susceptibility to illnesses. Consequently, infants and children often receive vaccinations and antibiotics to prevent severe infections like pneumonia.
5. Delayed growth or puberty: Insufficient oxygen and nutrients from impaired red blood cells can hinder growth in children and delay puberty in teenagers.
6. Vision problems: Sickle cell blockages in the small blood vessels supplying the eyes can damage the retina, causing vision impairment.
What are the complications of sickle cell anemia?
Sickle cell anemia can result in various complications, including:
1. Stroke: Blockage of blood flow to the brain by sickle cells can lead to a stroke, characterized by symptoms such as seizures, weakness or numbness in limbs, speech difficulties, and loss of consciousness. Immediate medical attention is necessary if these signs occur, as a stroke can be fatal.
2. Acute chest syndrome: Lung infections or blockage of lung blood vessels by sickle cells can trigger this life-threatening condition, presenting symptoms like chest pain, fever, and breathing difficulties, requiring urgent medical intervention.
3. Avascular necrosis: Blood vessel blockage by sickle cells can impair blood supply to bones, causing joint narrowing and bone death, most commonly affecting the hip joint.
4. Pulmonary hypertension: Adults with sickle cell anemia may develop high blood pressure in the lungs, manifesting as symptoms such as shortness of breath and fatigue, with potential fatal outcomes.
5. Organ damage: Sickle cell blockages in blood vessels deprive organs of oxygenated blood, leading to nerve and organ damage, including the kidneys, liver, and spleen, which can be life-threatening.
6. Splenic sequestration: Sickle cell accumulation in the spleen can cause enlargement, resulting in left-sided abdominal pain and posing a life-threatening risk.
7. Blindness: Blockage of tiny blood vessels supplying the eyes by sickle cells can progress to blindness over time.
8. Leg ulcers: Painful open sores on the legs can develop due to sickle cell anemia.
9. Gallstones: Breakdown of red blood cells produces bilirubin, contributing to gallstone formation.
10. Priapism: Painful, prolonged erections, known as priapism, can occur due to sickle cell blockage of penile blood vessels, potentially leading to impotence.
11. Deep vein thrombosis: Increased clotting risk from sickled red blood cells heightens the likelihood of deep vein thrombosis or pulmonary embolism, which can cause severe illness or death.
12. Pregnancy complications: Sickle cell anemia raises the risk of hypertension, blood clots, miscarriage, premature birth, and low birth weight in pregnant individuals.
How is sickle-cell anemia diagnosed?
A blood test can be conducted to detect the presence of abnormal hemoglobin associated with sickle cell anemia.
For adults, a blood sample is typically drawn from a vein in the arm, while in young children and infants, the sample is usually obtained from a finger or heel. The collected sample is then sent to a laboratory for screening to identify the sickle cell form of hemoglobin.
If sickle cell anemia is confirmed, additional tests may be recommended by your healthcare provider to assess potential complications associated with the condition.
In cases where individuals are carriers of the sickle cell gene, referral to a genetic counsellor may be advised for further evaluation and counselling.
When to see a doctor
If you or your child experiences symptoms of sickle cell anemia, such as fever or signs of stroke, it's crucial to seek immediate medical attention.
Infections can pose serious risks, especially for individuals with sickle cell anemia, as they are more susceptible. If a fever exceeds 101.5 degrees Fahrenheit (38.5 degrees Celsius), it's important to consult a healthcare professional promptly.
Symptoms of stroke warrant emergency medical care and include:
- One-sided paralysis or weakness in the face, arms, or legs.
- Confusion.
- Difficulty walking or speaking.
- Sudden vision changes.
- Unexplained numbness.
- Severe headache.
What is the treatment of sickle cell anemia?
Allogeneic stem cell transplantation is currently the sole curative option for sickle cell anemia and other variants of sickle cell disease. Typically, healthcare providers advocate for transplantation in cases where individuals experience severe complications like stroke, acute chest syndrome, or acute pain episodes.
As for treating sickle cell anemia, healthcare providers commonly employ strategies such as blood transfusions, antibiotics to address infections, and medications to alleviate symptoms arising from complications associated with sickle cell anemia.
FAQS
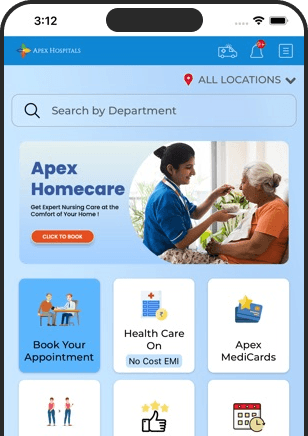
Health In A Snap, Just One App.
KNOW MORE