Celiac disease
What is Celiac disease?
Celiac disease is a hereditary autoimmune condition characterized by a response in the body to gluten, a protein found in certain grains. When gluten enters the digestive system, it stimulates the immune system to produce antibodies against it. These antibodies then attack the lining of the small intestine, known as the mucosa. As a result, the mucosa becomes damaged, reducing the ability to absorb nutrients from food, ultimately resulting in nutritional deficiencies.
How does celiac disease affect the body?
Celiac disease primarily affects the small intestine, the crucial site for nutrient absorption, including proteins like gluten. In individuals with celiac disease, gluten in the small intestine initiates an immune response. This response involves migrating inflammatory cells and antibodies to target and break down gluten molecules.
Consequently, the mucous membrane lining the small intestine, known as the mucosa, sustains damage.
The mucosa of the small intestine is intricately folded into numerous creases and finger-like projections called villi, which collectively provide a vast surface area for nutrient absorption. If extended, this surface area would span the size of a tennis court.
However, in individuals with celiac disease, immune cells triggered by gluten consumption gradually erode and flatten these projections, reducing the effective surface area available for nutrient absorption during digestion.
### What are the causes of celiac disease?
Numerous autoimmune conditions, including celiac disease, have a genetic component, meaning they are partly inherited disorders. This implies that a specific gene mutation transmitted through family lines increases the susceptibility to developing the condition. However, it's important to note that not everyone carrying the gene mutation manifests the disease, and not all individuals who develop the condition possess one of the identified genes. Other factors seem to play a role in triggering the onset of the disease.
What are the risk factors of celiac disease?
Celiac disease is more prevalent among individuals with
1. A family history of celiac disease or dermatitis herpetiformis.
2. Type 1 diabetes.
3. Down syndrome, William syndrome, or Turner syndrome.
4. Autoimmune thyroid disease.
5. Microscopic colitis.
6. Addison's disease.
What are the symptoms of celiac disease?
Symptoms of celiac disease can vary significantly and may differ between children and adults. In adults, digestive symptoms may include:
- Diarrhoea
- Fatigue
- Weight loss
- Bloating and gas
- Abdominal pain
- Nausea and vomiting
- Constipation
However, more than half of adults with celiac disease experience symptoms unrelated to the digestive system, such as:
- Anaemia, typically due to decreased iron absorption
- Loss of bone density (osteoporosis) or softening of bones (osteomalacia)
- Itchy, blistering skin rash known as dermatitis herpetiformis
- Mouth ulcers
- Headaches and fatigue
- Nervous system impairment, including numbness and tingling in the hands and feet, potential balance issues, and cognitive decline
- Joint pain
- Reduced spleen function (hypersplenism)
- Elevated liver enzymes
In contrast, children with celiac disease are more likely to exhibit digestive problems, including:
- Nausea and vomiting
- Chronic diarrhoea
- Swollen belly
- Constipation
- Gas
- Pale, foul-smelling stools
Nutrient malabsorption in children may result in:
- Failure to thrive in infants
- Damage to tooth enamel
- Weight loss
- Anaemia
- Irritability
- Short stature
- Delayed puberty
Additionally, children may experience neurological symptoms such as attention-deficit/hyperactivity disorder (ADHD), learning disabilities, headaches, lack of muscle coordination, and seizures.
Complications of Celiac disease:
Untreated celiac disease can result in various complications:
1. Malnutrition: If the small intestine fails to absorb sufficient nutrients, malnutrition may occur, leading to anaemia and weight loss. In children, malnutrition can stunt growth and result in short stature.
2. Bone weakening: Malabsorption of calcium and vitamin D in children can cause bone softening, known as osteomalacia or rickets. In adults, it may lead to decreased bone density, termed osteopenia or osteoporosis.
3. Reproductive issues: Malabsorption of calcium and vitamin D can contribute to infertility and miscarriage.
4. Lactose intolerance: Damage to the small intestine can cause abdominal discomfort and diarrhoea after consuming dairy products containing lactose. Once the intestine heals, tolerance to dairy products may improve.
5. Cancer risk: Individuals with untreated celiac disease have an elevated risk of developing various cancers, including intestinal lymphoma and small bowel cancer.
6. Nervous system disorders: Some individuals with celiac disease may develop neurological conditions such as seizures or peripheral neuropathy, a nerve disorder affecting the hands and feet.
When to talk to the doctor:
If you experience prolonged diarrhoea or digestive discomfort lasting more than two weeks, it's essential to consult your healthcare provider. Likewise, suppose your child exhibits the following symptoms. In that case, it's advisable to seek guidance from their healthcare team:
- Paleness
- Irritability
- Failure to thrive or grow
- Abdominal distension (potbelly)
- Bulky, foul-smelling stools
Before considering a gluten-free diet, it's essential to consult your healthcare team. Altering your gluten intake before celiac disease testing can impact the accuracy of test results.
Given the hereditary nature of celiac disease, it is prudent to discuss testing with your healthcare provider if a family member has the condition. Additionally, individuals with risk factors such as type 1 diabetes should inquire about celiac disease testing with a member of their healthcare team.
FAQS
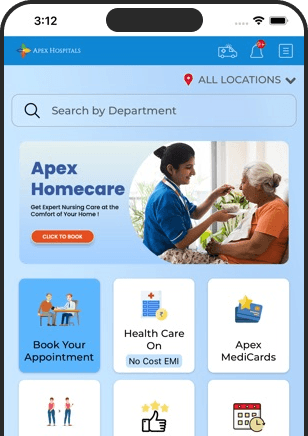
Health In A Snap, Just One App.
KNOW MORE