What is a nerve conduction study?
A nerve conduction study (NCS) is a diagnostic evaluation of the function of your peripheral nerves. NCS aids in detecting the presence and severity of peripheral nerve injury. Peripheral nerves are outside the brain and spinal cord (central nervous system).
In particular, an NCS measures the electrical current movement through:
- Motor nerves are the nerves responsible for controlling muscles and movement.
- Sensory nerves transmit information about touch, taste, scent, and sight to the brain.
If you experience symptoms such as tingling or numbness in your arms, legs, hands, feet, or face, your doctor may recommend an NCS. Depending on the situation, you may have the study in an outpatient setting or as part of your stay in a hospital. Typically, an NCS is performed alongside an EMG (electromyography) examination.
What is diagnosed by a nerve conduction study?
Nerve conduction investigations aid in the diagnosis of peripheral nerve disorders, particularly peripheral neuropathy and nerve compression syndromes. They can assist medical professionals in determining the cause, severity, and prognosis of these conditions.
- Peripheral neuropathy
When peripheral nerves are damaged, peripheral neuropathy occurs. Multiple conditions can result in peripheral neuropathy, which can affect various areas of the body depending on how and why it happens.
The following are prevalent causes of peripheral neuropathy:
- Diabetes mellitus.
- Nutritional deficiencies.
- Thyroid gland.
- Alcohol dependence disorder.
- Certain autoinflammatory disorders, such as lupus, rheumatoid arthritis, Sjogren syndrome, vasculitis, and Guillain-Barré syndrome
- Viral infections, such as HIV, or bacterial infections (such as Borrelia burgdorferi, which causes Lyme disease).
- Medication, including chemotherapy.
- Direct nerve damage caused by trauma or surgery.
- Nerve compression Syndrome
A nerve compression syndrome can occur when a peripheral nerve is compressed. It could result in peripheral neuropathy.
The following are examples of nerve compression syndromes:
- Carpal tunnel syndrome
- Sciatic nerve pain.
- Radial tunnel syndrome.
- Thoracic outlet syndrome.
- Meralgia paresthetica
What is the difference between an EMG and a nerve conduction study?
Neurologists frequently execute an EMG (electromyography) test and a nerve conduction study in the same setting, even though they are distinct tests. An EMG measures the amount of electrical activity produced by a muscle contraction. An NCS evaluates the passage of electrical current through a peripheral nerve before it arrives at the muscle. Additionally, it can detect the electrical activity of sensory nerves.
When providers perform these tests concurrently, they can determine whether your symptoms are due to a muscle disorder or a nerve problem.
How does nerve conduction testing function?
Like cables, nerves transmit electrical impulses or signals between the brain and the rest of the body. These impulses enable sensations and muscle movement. A nerve conduction study examines the transmission of these signals, mainly their speed and "strength."
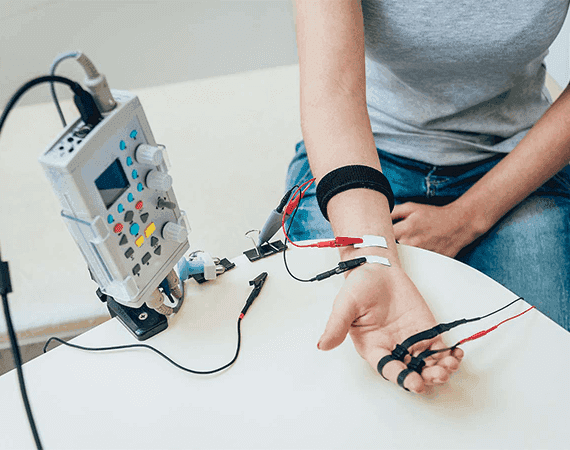
Along a nerve pathway, wires (electrodes) are taped to your skin at specific locations for this investigation. The nerve is stimulated with a modest electrical shock. The electrodes document the electrical current and its velocity as it travels down the nerve. If a motor nerve is enabled, the provider measures the response of the muscle it controls. The answer is recorded elsewhere along the nerve if a sensory nerve is stimulated.
Electrical signals in healthy nerves can travel up to 120 miles per hour. The current will be delayed and weaker if your nerve is damaged. By stimulating the nerve in multiple locations, the provider can determine the precise location of the nerve injury or problem.
How should I get ready for a nerve conduction study?
Before undergoing a nerve conduction study, you need to:
- Shower and wear loose-fitting, comfortable apparel.
- Avoid applying lotion, cream, and perfume to your epidermis. Creams and lotions can affect the integrity of a test.
- Inform the provider if you have a pacemaker or any other electrical medical device.
What can I expect from a nerve conduction study?
The procedure for a nerve conduction study can vary depending on the purpose of the test and the nerves being evaluated. In general, however, the following can be expected during a nerve conduction study:
- You will either recline or lie down for the exam.
- A healthcare professional will attach electrodes to your epidermis above the nerves they evaluate.
- They will affix various electrodes to the muscle or skin controlled by the nerves.
- The provider will then administer a small electrical impulse to your nerves, transmitting a signal to the controlled muscle. You may experience a mild tingling sensation.
- They will record the time required for your muscle or epidermis to react to the nerve signal.
- Then, they will replicate the same procedure in the next nerve until they have collected sufficient data.
- After the nerve conduction study, providers typically perform an EMG test.
How uncomfortable is a nerve conduction test?
The electrical stimulation may initially startle you, but it should not be painful. The jolt resembles a static electricity shock or may feel like a mild tingling. Most individuals can accomplish the test without difficulty.
How long does a study of nerve conduction last?
A nerve conduction investigation can range from 15 minutes to over an hour. It depends on how many nerves your physician examines.
What risks are associated with a nerve conduction study?
In general, nerve conduction investigations are safe. Electrical pulses may be uncomfortable, but the sensation should be fleeting and not painful.
FAQS
Health In A Snap, Just One App.
KNOW MORE
